The Impression/ Conclusion is probably the most important part of the report. It is the one portion of the report which would almost certainly be read by both the patient and the treating physicians. Busy physicians may unfortunately not find the time to read the entire findings section of the report, and often go directly to the impression. Hence, if there is one thing every radiologist must focus on in the report, it is this section. After the previous blog on anatomy of the radiology report, I am sharing a few tips and examples to how to write a good concise impression. Please note that most examples are either taken from my residents’ provisional reports while I am editing them (they are my guinea pigs for this blog!), or from anonymized outside reports. No offence is meant to anyone; I just feel it is easier to discuss these concepts with actual examples.
1. Answer the bloody question!
Every patient is sent for a study with one or few specific questions, and it is our job to answer these in the impression. While this should be an obvious dictum, it is unfortunately not always followed.
In The Hitchhiker’s Guide to the Galaxy by Douglas Adams (a must-read science fiction novel), an enormous supercomputer named Deep Thought is created to find the “Answer to the Ultimate Question of Life, the Universe, and Everything”. Deep Thought takes 7.5 million years to calculate the answer, which it then spurts out. The answer is ‘42’! This mystifies and frustrates all the characters, as no one understands the answer. Our impression should never read like ‘42’ to the referring physician.

For example, here is the impression of a patient with history of breast cancer and backache. The question obviously is whether there is metastatic recurrence causing the backache. The provisional impression created by my resident simply describes the presence of a compression fracture, without stating whether it is a benign compression fracture or metastatic. This makes the radiologist redundant. A technician could have done the MRI and the referring physician (or for that matter the technician as well) would have also easily picked the fracture from the MRI plates; where has the radiologist added any extra value to the report?

Another example. This is a successfully treated patient of retroperitoneal germ cell tumor on annual surveillance. The question asked simply is whether there is recurrent disease or not. However, the provisional impression does not answer that question at all. Instead, it reiterates two findings which have been there unchanged since the past few years. The ideal impression should read ‘CT reveals no evidence of recurrent or metastatic disease. Known situs inversus and treatment-related chronic IVC occlusion with associated collaterals are unchanged.’
2. Tell them what you think
Do not give non-specific descriptions in the impression; tell them what you think about the findings. Too often I see impressions which do not clarify what the findings represent, confusing the patients and the referring doctors alike. So do not simply put ‘sclerotic bone lesion’ in the impression in a patient with Ca lung; state whether it is most likely a bone island or is it suspicious for metastasis. Similarly, do not put ‘Prominent portocaval and retroperitoneal nodes’ in the impression (I see this all the time in patients with GI cancers); state whether you feel they are normal or infective or metastatic.
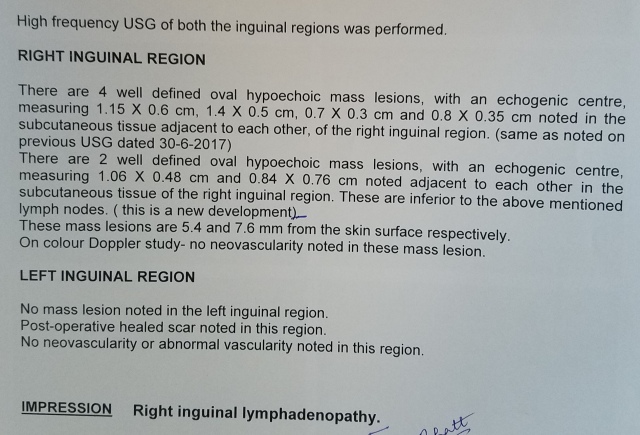
Here is an example of a patient with vulval cancer on surveillance (the most common site of metastatic recurrence is inguinal nodes). An outside USG report mentions ‘Right inguinal adenopathy’ as the impression. However, whether the radiologist thinks that this is benign or metastatic is not mentioned, making this a completely useless report. The patient panicked and came to Tata, where we redid the USG, which showed normal sized nodes (even the description of the nodes in the findings section of the outside report demonstrates them to all be subcm in short axis), with no suspicion for metastasis.
3. Do not give more image descriptors; state the pathology directly
Often, impressions include detailed image descriptors already there in the Findings section. Remember that the person reading the report is most likely not a radiologist and is not interested in nor understands radiology jargon. This only adds to the length of the impression, without adding any value. So cut down on imaging lingo and instead write clinically meaningful and actionable information in the impression using as few words as possible. Simply put, get to the point quickly in the impression, as eloquently put by Peter Kranz.

For example, my resident has here nicely stated the presence of a filling defect in the left femoral vein in the Impression, a great pick-up. Wouldn’t it be better however to simply state that there is a partial left femoral vein thrombus, rather than give an image descriptor as an impression?
4. Keep it concise and clear
To repeat Mark Twain’s famous words from the last blog on Anatomy of a radiology report: ‘I didn’t have time to write a short letter, so I wrote a long one instead.’ Keep the impression concise and to the point. A long wordy impression will help nobody and probably only add to the confusion, besides the chance of someone misinterpreting or missing an important finding hidden in the 15-line impression. Personally, I often find that giving 15 seconds extra to word the impression better also makes my thoughts on the report and on what should be done next for the patient clearer.

For example, the long impression in this outside report appears completely unreadable just because of its length. The radiologist could have said that ‘there is gastroduodenal and hepatic flexure thickening along with prominent locoregional and retroperitoneal nodes and mild mesenteric inflammation; the process appears to be tuberculous in etiology, with lymphoma being a less likely differential’, or something to that effect, in a much shorter manner if s/he gave some time to write a separate impression rather than just copying pasting the findings again.
5. Avoid hedging or giving too many differentials when you know what the diagnosis is
a. ‘4 cm peripherally enhancing hepatic mass; neoplastic etiology must be considered although other differentials like abscess, atypical hemangioma, or adenoma need to be ruled out. Clinical correlation suggested.’ Many radiologists write such impressions, despite knowing that the mass looks malignant, and is not a hemangioma and that the patient has no fever.
Compare this with ‘4 cm peripherally enhancing hepatic mass, consistent with malignancy. Other differentials like infection or benign neoplasm are considered unlikely.’
Or simply ‘4 cm peripherally enhancing hepatic mass, consistent with malignancy. A USG-guided biopsy is feasible and is recommended for further evaluation’.
I would personally prefer the 3rd or the 2nd impression to the first one.
b. Similarly, do not hedge regarding negative results either. For example:
‘No definite fracture or intracranial hemorrhage seen in this patient with head trauma’ can also be written without the ‘definite’, and ‘No suspicious lung nodules seen in this patient with pancreatic cancer’ can also be written as ‘No lung metastases’.
c. A tip; try using the word normal more often in the Impression. So if a patient with chronic cough has a normal CT chest, add a ‘Normal CT study’ or ‘Lungs are normal. No infection.’ to your impression rather than just ‘No significant abnormality seen’. Any person would prefer being called normal than ‘not abnormal’!
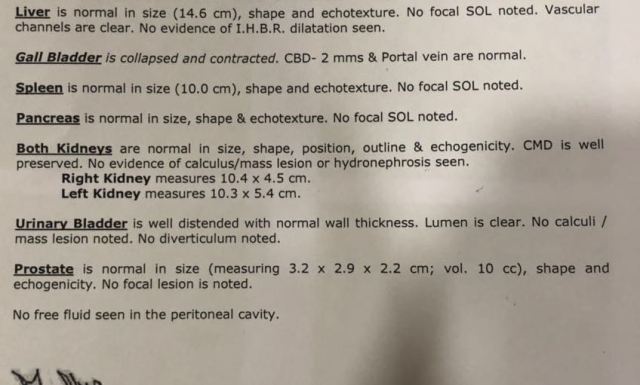
For example, this is my nephew’s USG report (he had hepatitis A). The radiologist did not write an impression at all! His parents freaked out reading that the gall bladder is contracted, thinking that this is an abnormal finding, and called me up immediately. A simple one phrase impression as ‘Normal abdominal ultrasound’ would have avoided a lot of needless apprehensions. Needless to say, they are not going to go to that radiologist again!
d. Finally, use words like ‘indeterminate’ if you cannot be sure of the diagnosis. So a single 4 mm pulmonary nodule in a patient with rectal cancer (note that this is statistically more likely to be benign) should be stated as ‘Indeterminate 4 mm pulmonary nodule, too small to characterize and needs to be followed-up after 3 months to rule out metastasis’ rather than directly calling it metastasis and confusing everyone. A larger 7-8 mm nodule can also be called indeterminate, with a recommendation for biopsy rather than short-interval follow-up given the higher likelihood of it being metastasis.
Here is an example of a right upper lobe 8 mm nodule (left image) in a patient with pancreatic cancer. Deemed metastatic on the outside report, we called it indeterminate and recommended biopsy (this was the only site of potential metastasis). The nodule had shrunk to 4 mm at the time of the biopsy (right image); we called off the biopsy and called it benign!

In contrast, this 8 mm nodule in a patient with colorectal cancer was indeed metastatic, demonstrating uptake on PET/CT (which also showed an additional bone lesion).
6. Avoid abbreviations and symbols in the impression
Remember that in this age of WhatsApp and email, the report may be seen by multiple doctors in different health set-ups and of different qualifications, as also by the patient and relatives. Abbreviations which you may consider standard in your set-up need not be standard or understood elsewhere.
a. For example, the term IHBRD/IHBD is ubiquitously used in India for intrahepatic biliary dilatation. However if an affluent patient emails this report to someone in the US for a second opinion, no one will understand what it means. No one uses this term in the US (they say no biliary dilatation instead of no IHBRD) and I used to always meet blank faces whenever I used this term while discussing a patient during my US stint. Ditto for ‘plain CT’; it is ‘non-contrast CT’ there.
b. Similarly, the term ITF (infratemporal fossa) or PFS (pyriform sinus) is often used in Tata for head and neck cancer patients, but putting it in the impression will be confusing for others, unless the full term is first introduced along with the abbreviation somewhere in the body of the report.
c. Avoid abbreviations like ‘e/o’ or ‘d/d’; patients do not understand this. Write ‘evidence of’ or ‘differentials’ instead.
d. Apart from abbreviations, avoid using query/question mark in the impression or indeed anywhere in the report. I have had many acquaintances or patients call me and read out their impressions as ‘Right ovarian cyst question mark benign’ asking me what it means. Worse still, others call with a ‘Right hepatic lesion question mark malignant question mark question mark abscess’ (‘Right hepatic lesion ?malignant ??abscess’). I often wonder whether the two ?? makes it a less likely differential than a single ? or more likely a differential!

For example, this is an outside ultrasound report of an acquaintance which talks of a small right ovarian cyst, and states ‘nature ? benign’. What should a patient understand from this report? Read the next line: ‘Associated minimal right pleural effusion’. Is pleural effusion associated with a benign functional ovarian cyst? In fact, it is associated with an ovarian neoplasm! This is a classic example of not giving those extra 10 seconds to phrase the report better by removing the word ‘associated’. The two findings were completely unconnected in this case. Furthermore there is no recommendation of what to do next, whether there is a follow-up USG required or not, and at what time interval. Instead, the radiologist writes the famous tagline ‘Ad clinical correlation’! (At least use ‘Adv’ as an abbreviation for advice if you are too lazy to type the entire word!)
7. Non-specific findings: Leave them from the impression or clarify that they are nothing to worry about
We often see many non-specific or incidental findings in a patient’s scan, be it degenerative spinal changes or brain white matter hyperintensities or a small thyroid nodule. If there is nothing to worry about them, nor anything which requires follow-up, I would suggest not including them in the impression. Either ways, make sure that you clarify that they are not clinically significant in the Findings section or the Impression. Jenny Hoang has a nice article on this in JACR.
For example, describe ‘Non-specific white matter hyperintensities in the brain’ as ‘age-appropriate’ or ‘of no clinical significance’ in the findings and leave it there. If you insist on putting it in the impression, pleas again clarify it similarly, as Dr Google will give frightening differentials of white matter hyperintensities to the patients.
8. Recommend completely when it comes to radiology-related recommendations
The most common question in the patient’s or doctor’s mind after reading the radiology report usually is ‘what next?’. Hence, providing appropriate recommendations is important. However, always ensure that the recommendation is complete and not vague.
a. You will often recommend a biopsy or an FNA (or simply ‘tissue sampling’) for a lesion. Be sure to specify whether you are recommending a USG-guided sampling or a CT-guided sampling. Conversely, if you see a 3 mm indeterminate pulmonary nodule in a patient with cancer, apart from stating that it is indeterminate, also clarify that it is not amenable to biopsy due to its small size or location.
b. Avoid vague terms like ‘short-term follow-up’; does that mean 4 weeks, 8 weeks, or 6 months? For example, for the above indeterminate nodule, you may state that ‘follow-up non-contrast CT chest recommended after 8-12 weeks.’
c. If there is a guideline or criteria or paper based on which you are making a recommendation, state so. For example,
‘6 cm simple left ovarian cyst in this premenopausal woman; a follow-up USG at 6-12 weeks recommended as per American College of Radiology (ACR) guidelines.’
‘5 mm incidental right pulmonary nodule; follow-up CT at 12 months recommended in this low risk patient as per Fleishner society guidelines’
Conversely, you can also write ‘8 mm incidental left thyroid nodule; this does not require further evaluation as per ACR guidelines.’
d. ‘Clinically correlate’ should be avoided in most cases for many reasons. We are clinicians too and can correlate most findings, or call the referring physician to clarify history if needed. Furthermore, we do not need to ask the referring physician to clinically correlate; s/he is bound to do so anyway even if we do not put it in the impression!
As a general rule, I try using this term in less than 10% of my reports. An example of exceptions could be ‘Right C5/6 foraminal stenosis along with severe lower cervical canal stenosis; needs clinical correlation regarding the neurological level of the patient’s symptoms’, if we are unable to find exact examination details.

Here is a particularly inexcusable example of what I mean; read the impression of a positive outside lower limb Doppler study. An acute DVT is an acute DVT on USG; there is no differential or doubt about it. What is the need of suggesting clinical correlation in this case? This is just a mechanical spinal level statement made by an otherwise competent radiologist who has made the correct diagnosis, but leads to a poor impression about the entire radiology community in the minds of the referring physicians.
9. Document communication of critical findings
As a doctor, it is important to communicate urgent findings like pneumothorax or pneumoperitoneum immediately to the referring physician. Medicolegally, it is equally important to document this communication. So if you see a patient with say pulmonary embolism and call the referring physician to convey the findings, add a line after the impression which states ‘The critical finding of pulmonary embolism was communicated by Dr ABC to Dr XYZ at 12.30 pm on 5.5.18’.
10. Proof-read for grammar, syntax, and lucidity of report
As I said, the Impression is what is read the most, so the way you word the Impression in the report is also what creates your impression as a competent radiologist in the minds of the doctor and the patient. So always proof-read and double check the impression. Spelling mistakes and grammatical errors leave a poor impression on the referring doctor.
One general convention in the grammar or syntax context of the impression is that you need not write ‘is seen’ or ‘is noted’ in the impression. So, instead of writing ‘3 mm right upper lobe pulmonary nodule is seen; follow-up CT is recommended after 3 months’, you can simply write ‘3 mm right upper lobe pulmonary nodule; follow-up CT recommended after 3 months.’ Another example: instead of writing ‘There is a right upper lobe spiculated mass, suspicious for malignancy’, you can write ‘Right upper lobe spiculated mass, suspicious for malignancy’.

To culminate, here is an example of a classic ’42’ as the radiology report; a particularly poor radiology impression (it was a provisional report of a 2nd year resident, so we can forgive him!). This is a patient of medulloblastoma on surveillance. The question asked is whether there is recurrence of not, which is not answered in the impression. Instead, a vague description of an altered right cerebellar altered intensity is given, which would scare any patient/parent and many doctors as well. These were just post-treatment gliotic changes. This is followed by a convoluted description of an occipital microhemorrhage, which is related to the past surgery/radiation. To top it all, the spelling of cerebellum is wrong. A simple impression would be ‘MRI reveals expected post-treatment changes. No evidence of recurrent disease.’
These are few general rules to help radiologists write a concise, lucid, and helpful impression (mark all three adjectives; they are equally important). These are of course my own views, and everyone’s opinions are welcome in the comments section!
-Akshay Baheti, Tata Memorial Hospital
PS: I have not talked about giving addendums to already issued reports (instead of changing the impression and reissuing a ‘fresh’ report) in this section, because of copyright issues. Suffice to say, once a report is issued, if you want to change any part of the body or impression, you should issue an addendum rather than change/edit the report and issue a ‘new’ one. This is discussed in detail in a dedicated chapter in a book co-authored by Dr Bhavin Jankharia and me on practical radiology issues, titled Known Unknowns of Every Radiology Practice. It is available on Amazon and on the REF website by clicking on the links.




I agree with most of what you have said.
But, I as have said before. reports are not meant for PATIENTS to read . They are meant to be read by the referring physician and explained to the patient. If patients read the reports and start worrying – worse still Google, it is not our fault – though is still a matter of concern to us. And, unlike lab reports , radiology reports often and necessarily have shades of gray and is everything is not always written in stone. Often, I have wondered if radiology reports should be handed over in sealed envelopes to patients.
LikeLike
If patients follow what they are supposed to follow Sir, I wouldn’t be needing to remind my wife to take her antihypertensive medications every night! I feel that, particularly in India where there is no certainty of how well the referring physician will counsel the patient about his/her condition and where whatsapp consults for various reports and medical conditions are common, we will have to assume that the patient will read the report and try to understand or google more about it if something doesn’t make sense to him/her.
LikeLike
Pingback: The Art and Science of Radiology Reporting – Cafe Roentgen
Pingback: Anatomy of the Radiology Report – Cafe Roentgen
Pingback: The Findings (Body) of the Radiology Report: What to say and how to say it? – Cafe Roentgen
Pingback: Remove the query from your impression; literally! – Cafe Roentgen
Pingback: Remove the ‘query’ from your impression! It’s time for a lexicon for conveying certainty – Cafe Roentgen
A concise, lucid and helpful article 🙂 just like a good radiology report impression
LikeLiked by 1 person
really helpful and meaningful article
LikeLike
Great read!!! Thanks for sharing such a great blog with us. These blogs will really help us.
LikeLike